Thalassaemia in India: UPSC Current Affairs Notes [2025]
Dec, 2025
•7 min read
Why in the News?
- Thalassaemia has been in the news for the past month due to unsafe blood transfusions and HIV infection cases among thalassaemia patients.
- Renewed focus on blood bank regulation and screening standards.
- Demands for passing the National Blood Transfusion Bill, 2025.
Why Cover this Topic for UPSC?
- GS Paper II & III: public health, governance and health infrastructure.
- Current Affairs: blood safety, regulation and health policy reforms.
- Prelims: genetic disorder, transmission and prevention.
- Essay & Interview: Potential topic for health equity and policy implementation.
About Thalassaemia
Thalassaemia is a genetic blood disorder in which the body is unable to produce sufficient healthy haemoglobin, leading to chronic anaemia. It is an inherited condition, meaning it is passed from parents to children, and is not contagious.
In India, thalassaemia is a major public health concern due to a high number of carriers and the need for lifelong medical care in severe cases.
- Thalassaemia is caused by mutations in genes responsible for haemoglobin production.
- It mainly occurs in two forms: Alpha thalassaemia and Beta thalassaemia (more common in India).
- Severe cases require regular blood transfusions, leading to risks like iron overload and infections.
- The disease is preventable through carrier screening, genetic counselling and prenatal diagnosis.
- In 2023, a dedicated thalassemia module was integrated into the Sickle Cell Portal to enable states to enter records of existing thalassemia patients.
- As of July 2025, a total of 4,361 thalassemia patients have been registered nationwide on the sickle cell portal, with 2,579 of them being children under the age of 12.
- Effective management needs a safe blood supply, awareness and strong public health systems.
Types of Thalassaemia
Thalassaemia is broadly classified based on the type of haemoglobin chain affected and the severity of the disorder.
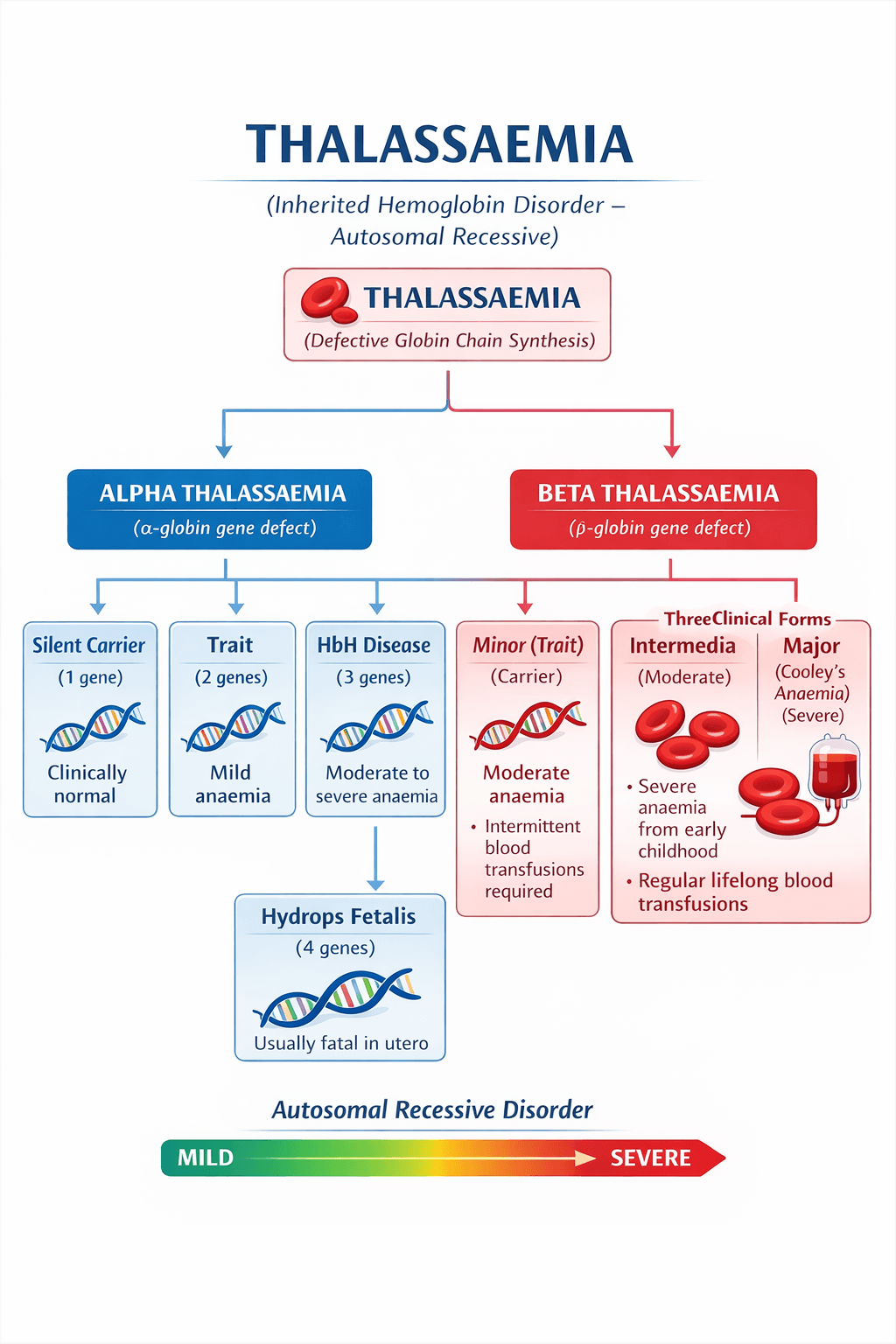
1. Alpha Thalassaemia: Alpha thalassaemia is a genetic blood disorder caused by reduced or absent production of alpha globin chains, an essential component of haemoglobin.
- Severity depends on the number of defective alpha-globin genes inherited.
- Mild forms may show no symptoms, while severe forms can cause serious foetal complications.
- Commonly detected through genetic screening and prenatal tests.
2. Beta Thalassaemia: Beta thalassaemia occurs due to defective synthesis of beta globin chains, leading to reduced haemoglobin and chronic anaemia. It is most common in India and is classified into three clinical forms:
- Beta Thalassaemia Minor (Trait): The Individual is a carrier with mild or no symptoms
- Beta Thalassaemia Intermedia: Moderate anaemia; intermittent blood transfusions required.
- Beta Thalassaemia Major (Cooley’s Anaemia): Severe anaemia from early childhood. Requires lifelong regular blood transfusions and iron chelation therapy.
Must read about: Tuberculosis in India: Types, Symptoms, Challenges & Elimination Strategy 2025
Symptoms of Thalassaemia
The symptoms of thalassaemia vary depending on the type and severity of the disorder. While carriers may remain asymptomatic, severe forms present early in childhood and require continuous medical care.
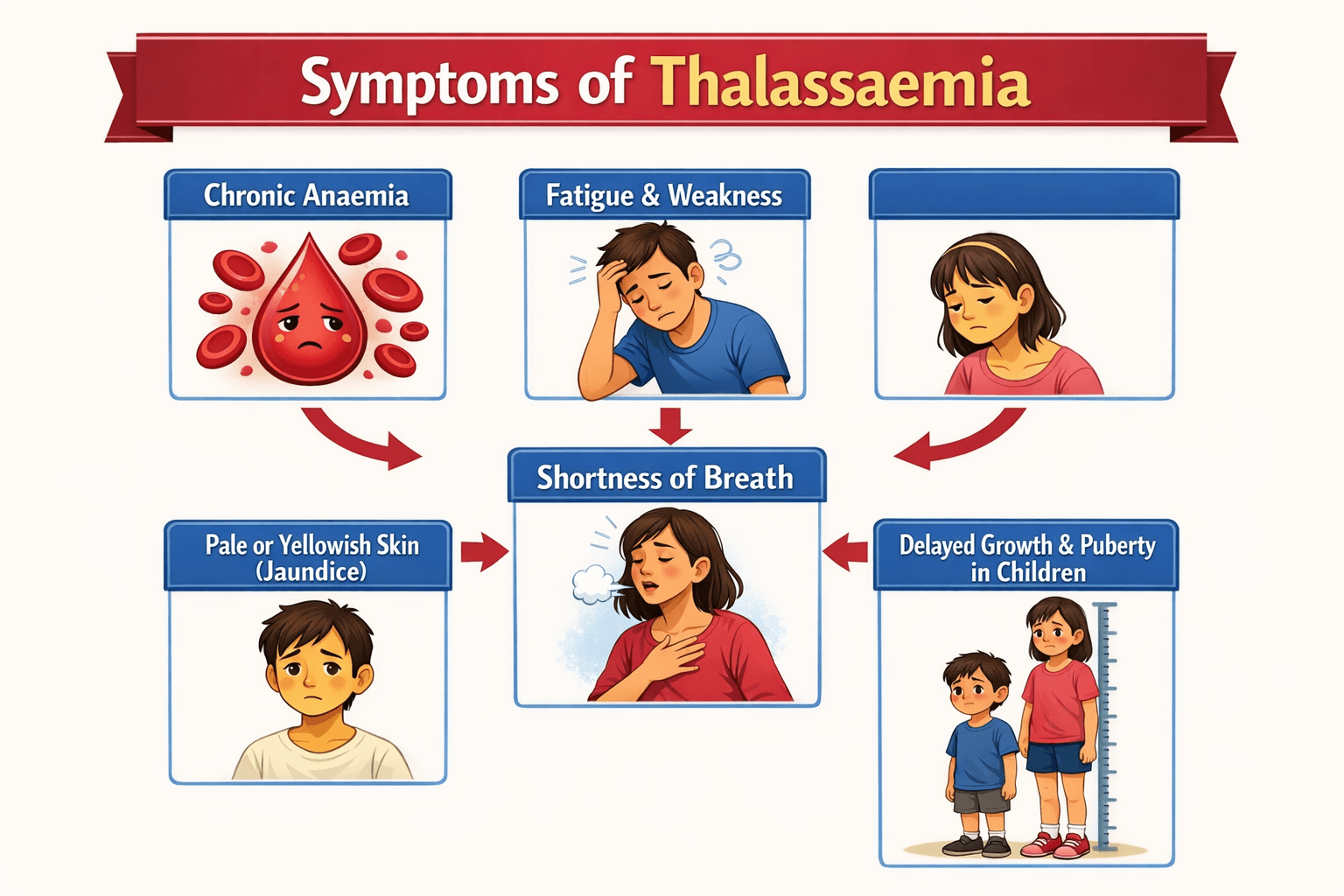
Symptoms in Moderate to Severe Thalassaemia
- Bone deformities, especially of the face and skull, are due to bone marrow expansion
- Enlarged spleen and liver (splenomegaly, hepatomegaly)
- Frequent infections due to weakened immunity
- Dark-coloured urine caused by excess breakdown of haemoglobin
Many symptoms arise not only from anaemia but also from repeated blood transfusions, leading to iron overload, which can damage the heart, liver and endocrine organs.
Also read: Indian Council of Medical Research (ICMR) | UPSC Notes
Treatment of Thalassaemia
The treatment of thalassaemia focuses on managing symptoms, preventing complications and improving quality of life, as there is no universal cure for all forms. The approach depends on the severity of the disease.
1. Regular Blood Transfusions:
- Essential for patients with thalassaemia major and severe intermedia.
- Helps maintain adequate haemoglobin levels but increases the risk of iron overload.
2. Iron Chelation Therapy:
- Used to remove excess iron accumulated due to repeated transfusions.
- Prevents damage to vital organs such as the heart, liver and endocrine glands.
3. Bone Marrow / Stem Cell Transplantation:
- Currently, the only curative treatment, especially effective in children.
- Limited by donor availability, high cost and procedural risks.
4. Supportive Care:
- Includes folic acid supplementation, management of infections and regular monitoring.
- Splenectomy may be advised in selected cases with severe splenomegaly.
5. Preventive Aspect:
- Carrier screening, genetic counselling and prenatal diagnosis are the most effective long-term strategies to reduce disease burden.
Must cover this key topic: AdFalciVax: ICMR Indigenous Vaccine for Malaria
UPSC Prelims PYQ on Diseases in News
QUESTION 1
GS
Medium
Science & Technology
Prelims 2025
With reference to monoclonal antibodies, often mentioned in news, consider the following statements:
I. They are man-made proteins. II. They stimulate immunological function due to their ability to bind to specific antigens. III. They are used in treating viral infections like that of Nipah virus.
Which of the statements given above are correct?
Select an option to attempt
Thalassaemia: Unsafe Blood Transfusions & HIV Risk
Thalassaemia has come into public focus in recent months due to reports of HIV infections among thalassaemia patients, allegedly caused by unsafe blood transfusions. A reported case from Kolkata highlighted how a thalassaemia patient contracted HIV during childhood due to repeated transfusions.
- Recent cases have shown that unsafe or poorly screened blood can transmit HIV, Hepatitis B and Hepatitis C to such patients.
- This shows that for thalassaemia patients, blood safety = life safety.
- Lapses in blood banks turn a genetic disorder into a lifelong dual disease burden.
Must read: National Organ and Tissue Transplant Organisation (NOTTO)
Government of India Initiatives on Thalassaemia
The Government of India follows a multi-pronged approach to tackle thalassaemia, focusing on prevention, early detection, safe blood supply and long-term treatment support. These initiatives are highly relevant for UPSC GS II (Health Governance) and GS III (Human Development & Public Health).
1. National Health Mission (NHM)
- Thalassaemia management is supported under the NHM framework, especially at district hospitals and medical colleges.
- NHM provides free or subsidised blood transfusions and basic diagnostics and follow-up care.
- Strengthens public health infrastructure, which is crucial for transfusion-dependent patients.
2. National Programme for Prevention and Control of Genetic Disorders (NPCGD)
- Specifically targets genetic disorders, including thalassaemia.
- Implemented in selected tertiary care hospitals and medical colleges. Key focus areas include:
- Carrier screening among adolescents and pregnant women
- Genetic counselling for at-risk couples
- Prenatal diagnosis to prevent the birth of affected children
3. Rashtriya Bal Swasthya Karyakram (RBSK)
- Screens children (0–18 years) for 4Ds: Defects, Diseases, Deficiencies and Developmental delays.
- Thalassaemia is included under diseases detected early in childhood.
- It enables early identification and referral to higher medical centres for long-term management.
4. National Blood Policy & Blood Transfusion Services
- Aims to ensure a safe, adequate and quality blood supply across the country.
- Mandates screening of all donated blood for HIV, Hepatitis B & C and Syphilis and Malaria
- Blood banks are regulated under the Drugs and Cosmetics Act, 1940.
Recent HIV cases among thalassaemia patients highlight implementation gaps in this policy.
5. Ayushman Bharat – Pradhan Mantri Jan Arogya Yojana (PM-JAY)
- Provides financial protection up to ₹5 lakh per family per year.
- It covers hospitalisation, diagnostics and management of complications related to thalassaemia.
- Reduces out-of-pocket expenditure for poor and vulnerable families.
6. Thalassemia Bal Sewa Yojana (TBSY)
- This scheme is implemented by the Union Health Ministry, in association with Coal India Limited (CIL).
- Financial assistance up to Rs 10 lakh is provided to eligible patients for Bone Marrow transplants (BMT) from CIL Corporate Social Responsibility (CSR) funds.
- This scheme provides for BMT in 17 empanelled hospitals spread across the country.
7. Awareness & Screening Initiatives
- Premarital and antenatal screening in high-prevalence regions.
- Awareness campaigns through World Thalassaemia Day (8 May).
- The theme of 2025 was “Together for Thalassaemia: Uniting Communities, Prioritising Patients.”
- Encourages voluntary blood donation to meet transfusion needs safely.
8. Support for Thalassaemia Day Care Centres
- Some states, with central support, run day care transfusion centres.
- These centres provide regular transfusions, monitoring for iron overload and counselling and follow-up care.
Also see: National Cancer Awareness Day 2025
The Way Ahead
A preventive, well-regulated and patient-centric approach is essential to reduce India’s thalassaemia burden and restore trust in the public healthcare system.
- Zero-tolerance on Unsafe Blood: Strict monitoring and accountability of all blood banks.
- Prevention Over Treatment: Nationwide carrier screening and genetic counselling.
- Better Access to Care: District-level thalassaemia centres and assured drug supply.
- Policy Integration: Mainstream thalassaemia under NHM and PM-JAY.
- Awareness & Donation: Promote voluntary blood donation and public awareness.
Prepare this important current topic here: What is Nipah Virus: Everything You Need to Know
Start your UPSC Preparation 2026/2027 with SuperKalam
SuperKalam is your personal mentor for UPSC preparation, guiding you at every step of the exam journey. Practice, revise, and evaluate– all in one place.
Download Now

