What is Nipah Virus: Everything You Need to Know
Jul, 2025
•5 min read
Why in the News?
The Nipah virus has claimed a second life in Kerala, triggering a high alert in six districts. As a precaution, 675 individuals have been added to the contact tracing list, raising serious public health concerns.
Why Cover This Topic for UPSC?
- For Prelims: Nipah virus origin, transmission, symptoms, & affected states.
- UPSC current affairs linked to public health and epidemic response
- GS Paper II: Governance, health policy, Centre–State coordination
- Reflects the roles of institutions like ICMR, NIV, and state health bodies
- Useful for Essay and Ethics: medical ethics, public safety, & policy response
What is Nipah Virus?
Nipah virus (NiV) is a highly infectious virus that spreads from animals to humans (zoonotic pathogens) and can also spread between people. It causes severe illness like brain inflammation (encephalitis) and respiratory problems, often leading to death.
- The Nipah virus belongs to the Paramyxoviridae family and the Henipavirus genus.
- According to the WHO, the virus has a high death rate, ranging from 40% to 75%, depending on the outbreak and healthcare response.
- It spreads through direct contact with infected animals, especially fruit bats or pigs, contaminated food (like half-eaten fruits), or close contact with infected people.
Origin of Nipah Virus
The virus was first identified during an outbreak in 1998–99 in Malaysia and Singapore, among pig farmers. Fruit bats (also called flying foxes) are the natural carriers of the virus and are believed to have passed it to pigs, which then infected humans. Since then, outbreaks have occurred mostly in South and Southeast Asia, including regular episodes in India (Kerala) and Bangladesh.
How Does Nipah Virus Spread?
Nipah virus (NiV) spreads from animals to humans and also between humans. The infection can happen through several routes, making it a serious public health concern.
Animal-to-Human Transmission
- Fruit bats (also known as flying foxes) are the primary carriers of the Nipah virus.
- Humans may get infected by consuming fruits or raw date palm sap contaminated by bat saliva or urine.
- In past outbreaks, pigs acted as intermediate hosts. The virus can pass to humans through direct contact with infected pigs or their bodily fluids.
Human-to-Human Transmission
- Spread occurs through close contact with an infected person's body fluids (saliva, urine, blood, etc.).
- High risk of transmission in healthcare settings due to exposure to infected patients without proper protective measures.
Symptoms of Nipah Virus
After infection, Nipah virus symptoms typically begin to show within 4 to 14 days. The virus primarily affects the brain and respiratory system. Symptoms can start mild but may progress rapidly to severe and even fatal complications.
Mild to Moderate Symptoms
These usually appear in the early phase of infection:
- Fever – Often the first sign, persistent and high-grade
- Headache – Throbbing pain due to viral impact on the nervous system
- Muscle pain (Myalgia) – General body ache and discomfort
- Sore throat and cough – Especially in early or respiratory-dominant cases
- Fatigue or drowsiness – Feeling unusually tired or sluggish
- Nausea or vomiting – Digestive symptoms in some patients
Severe Symptoms
These symptoms may develop rapidly within 1–2 days of the early signs:
- Breathing difficulties – Due to inflammation or infection in the lungs
- Seizures – Sudden and uncontrolled electrical disturbances in the brain
- Disorientation or confusion – Signs of brain involvement (encephalitis)
- Encephalitis – Inflammation of the brain; hallmark of severe Nipah cases
- Coma – In advanced stages, patients may slip into a coma within 24–48 hours of severe brain inflammation
Note: Some patients may show only respiratory symptoms, while others may develop neurological complications. The high fatality rate (40–75%) is largely due to the rapid onset of encephalitis.
How is Nipah Virus Diagnosed?
Early diagnosis of Nipah virus is critical, but it can be challenging because the initial symptoms resemble common illnesses like the flu or dengue.
1. RT-PCR (Real-Time Polymerase Chain Reaction): It identifies the virus’s genetic material in samples such as throat or nasal swabs, urine, or blood. This test is most effective in the initial stages of infection.
2. ELISA (Enzyme-Linked Immunosorbent Assay): For patients in later stages or retrospective diagnosis, ELISA is used to detect IgM and IgG antibodies against the Nipah virus in blood samples.
In India, diagnosis is primarily conducted by the National Institute of Virology (NIV), Pune, along with ICMR-approved VRDL (Virus Research and Diagnostic Laboratory) networks, all of which maintain the required biosafety protocols (BSL-3/4).
Treatment & Precautions to Prevent Nipah Infection
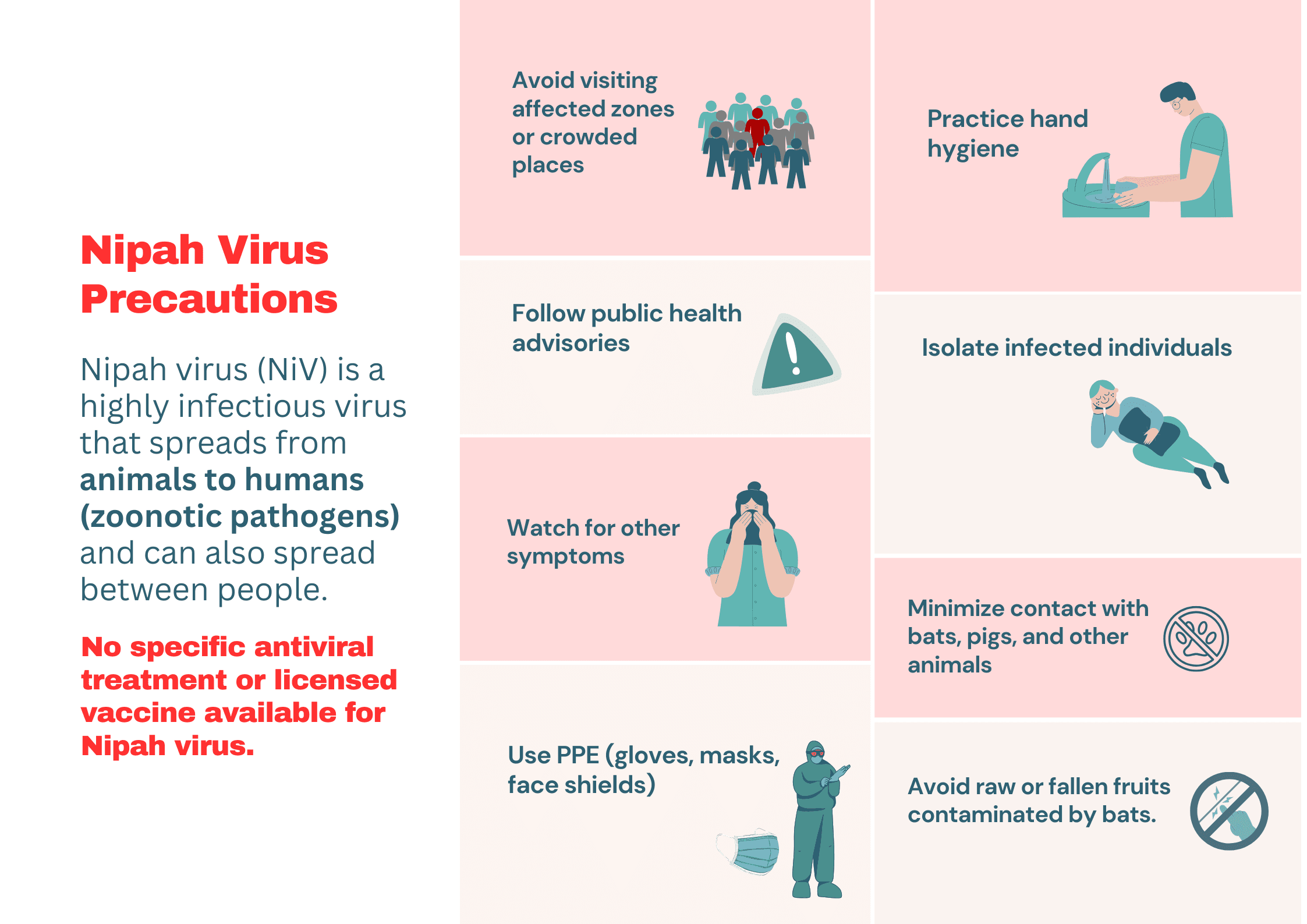
There is currently no specific antiviral treatment or licensed vaccine available for the Nipah virus. Management mainly focuses on supportive care and preventive actions to control the spread of infection. Early detection and isolation remain crucial to reducing fatality and transmission. Here are some essential precautionary measures:
- Avoid raw or fallen fruits and do not consume raw date palm sap, which may be contaminated by bats.
- Minimize contact with bats, pigs, and other animals, especially in outbreak-prone areas.
- Use PPE (gloves, masks, face shields) when dealing with suspected or confirmed cases.
- Isolate infected individuals and ensure proper sanitation in households and hospitals.
- Practice hand hygiene—wash hands frequently with soap and water.
- Avoid visiting affected zones or crowded places during outbreaks.
- Follow public health advisories issued by local authorities and the WHO.
Despite the presence of Nipah virus (NiV) antibodies in fruit bats across several Indian states, human outbreaks have remained concentrated in Kerala. Let’s understand the reasons behind this pattern.
Why Is Kerala the Epicentre of Nipah Virus Outbreaks in India?
The state has reported four outbreaks between 2018 and 2023, making it the most affected region in India for this deadly zoonotic disease. This repeated emergence in Kerala is not coincidental but is driven by a combination of ecological, geographical, and socio-behavioural factors.
1. Dense Fruit Bat Population: Kerala is home to a significant population of Pteropus medius (Indian flying fox), the primary natural reservoir of Nipah virus.
2. Favourable Climate and Ecosystem: The warm, humid, and forest-rich environment provides an ideal breeding ground for bats and other wildlife that carry zoonotic viruses.
3. Human-Wildlife Interface: High population density and human encroachment into forested areas increase the chances of spillover from bats to humans.
4. Agricultural Practices: Cultivation of fruit-bearing trees near human settlements allows bats to forage close to people. Consumption of partially eaten or fallen fruits increases infection risk.
5. Urban-Rural Connectivity: Kerala’s dense road networks and inter-district mobility may aid faster transmission compared to more isolated areas.
Although NiV antibodies have been found in bats across several other Indian states, no major human transmission has been reported outside Kerala. It is likely due to a combination of fewer spillover events and weaker surveillance elsewhere.
Also cover this recent topic: India’s First Transgender-Led Health Clinic: Sabrang Clinic in Hyderabad
How Has India Responded to Nipah Virus Outbreaks?
India has experienced multiple Nipah virus outbreaks since 2001, particularly in Kerala and West Bengal. Given the virus’s high fatality rate and potential for human-to-human transmission, the country’s response has evolved to become more swift, coordinated, and multi-level.
Containment and Surveillance Measures
- Rapid identification of index cases through community reporting and hospital alerts
- Contact tracing of high-risk individuals (675+ contacts traced in the recent outbreak)
- Isolation and quarantine of suspected and confirmed cases
- Sealing of affected zones and restriction of movement
- Declaration of containment zones in affected districts
Diagnostic Preparedness
- Deployment of mobile BSL-3 labs by ICMR-NIV in outbreak areas (e.g., Kozhikode, Kerala)
- Strengthening of the VRDL (Virus Research and Diagnostic Laboratory) network for real-time testing
- Prioritised testing using RT-PCR and ELISA for early detection
Healthcare Infrastructure and Crisis Management
- Setting up dedicated isolation wards and ICU support in district hospitals
- Protocols issued for clinical management and PPE use among healthcare workers
- Training sessions for frontline workers on Nipah-specific protocols
- Availability of ventilators and emergency medicines in high-alert zones
Public Awareness and Community Engagement
- Dissemination of government advisories in local languages
- Campaigns to avoid the consumption of fallen fruits and raw palm sap
- Community-based surveillance and sensitisation of ASHA workers, anganwadi staff, and local leaders
Institutional and Inter-Governmental Coordination
- Central monitoring by the Ministry of Health & Family Welfare
- Technical and operational support from ICMR, NIV, and the National Centre for Disease Control (NCDC)
- Support from the WHO and foreign experts during major outbreaks
- Kerala government’s proactive role in preparedness and district-level coordination
Research and Long-Term Strategy
- ICMR’s collaboration with global partners to develop monoclonal antibodies and vaccines
- WHO lists Nipah virus among the top priority diseases for R&D
- Surveillance of fruit bats and environmental samples under the “One Health” framework
Also read: India's Global Health Leadership: Achievements, Challenges, and Opportunities
Way Forward
The Nipah virus, like COVID-19, is a reminder that zoonotic diseases are not rare events but a growing public health concern. To avoid another large-scale health crisis, India must adopt a proactive, long-term strategy that integrates health, environment, and governance.
For UPSC aspirants, this topic reflects the role of future policymakers in designing integrated, preventive healthcare systems.
“A proactive policymaker is the first line of defence against the next pandemic”.
Prepare UPSC Current Affairs with SuperKalam
- Stay updated on global and national issues with our Daily News Analysis
- Practice mains answers with Instant Mains Answer Evaluation
- Build your study momentum with streaks and leaderboards
Explore SuperKalam's Resources and set yourself on the path to success!
UPSC Prelims PYQs
QUESTION 1
Hard
Science & Technology
Prelims 2023
Question: Consider the following statements: Statement I: India’s public sector health care system largely focuses on curative care with limited preventive, promotive, and rehabilitative care. Statement-II: Under India’s decentralized approach to health care delivery, the States are primarily responsible for organizing health services. Which one of the following is correct with respect to the above statements?
Select an option to attempt
QUESTION 2
Medium
Science & Technology
Prelims 2023
In the context of vaccines manufactured to prevent COVID-19 pandemic, consider the following statements:
- The Serum Institute of India produced COVID-19 vaccine named Covishield using the mRNA platform.
- Sputnik. V vaccine is manufactured using a vector-based platform.
- COVAXIN is an inactivated pathogen-based vaccine. Which of the statements given above are correct?
Select an option to attempt


